California Tells Hospitals to Push Back on ICE — What Nurses Need to Know
State officials are telling hospitals and clinics to protect patients and follow strict protocols when immigration agents show up. The catch: state rules meet federal limits, so your actions need to be precise.
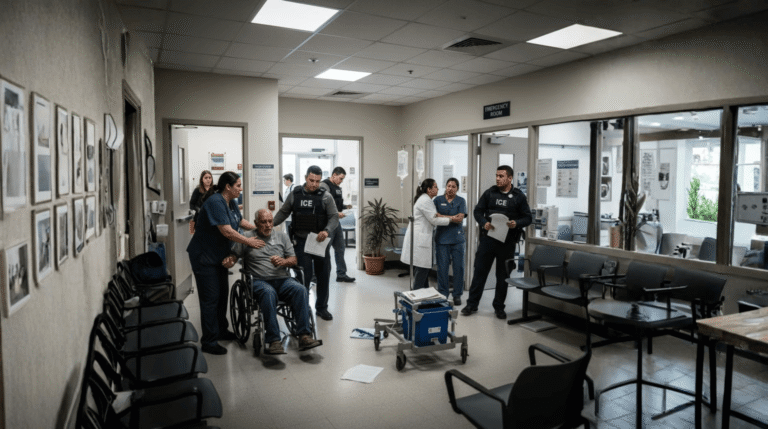
You’ve probably seen the stories: immigration officers near clinics, ERs, even street-medicine tents.
California now requires hospitals and clinics to set clear protocols for immigration enforcement requests. Patient immigration status and birthplace are treated like protected medical information. Staff are directed to route agents to designated administrators or legal counsel and keep nonpublic areas closed without a warrant or court order.
What happened?
Reports from across Southern California describe immigration agents appearing at medical sites, including a case where officers surrounded a street-medicine tent and others where detained patients were guarded in rooms. The state response is a new package of laws and guidance that clarifies what facilities can refuse and what requires a judge-signed order.
Why this matters
This is about safety, trust, and keeping care on track.
- Patients are more likely to show up when they know their info won’t be shared without a court order.
- Units stay calm when everyone follows one script for agent requests.
- Public areas are one thing, but exam rooms and most work spaces are not. No entry there without a judge-signed warrant.
So what exactly changed?
Let’s keep it simple.
- Status and birthplace = private, like medical records. Don’t disclose without a warrant or court order.
- If agents arrive or ask for records, call your unit’s point person or legal contact. Don’t handle it solo.
- Administrative warrants aren’t enough for entry. Nonpublic areas stay closed without a judicial warrant.
- More policy updates may come after court challenges, so expect refreshers.
Here’s What You Can Do Right Now
Here are some few steps you need to remember on shift.
- Keep caring for your patient
Don’t pause meds, vitals, or discharge just because an agent appears.
Say: “I’ll contact the administrator who handles requests like this,” then make the call and return to care.
- Control access to nonpublic areas
Units, pods, treatment rooms, and back halls are nonpublic.
If someone tries to step in, use: “This is a nonpublic area. Please wait here while I call our administrator.”
If they mention a warrant, ask them to show it to the designated contact.
- Don’t share information at the door or desk
No status, no room numbers, no diagnosis, no “yes/no” that a person is a patient.
Route all questions to the unit’s admin/legal contact. That’s their job.
- Document the encounter
Write down: time, location, what was requested, names or badge numbers if offered, and who you called.
Keep it short and factual. No opinions.
- Reassure the patient and family
Quiet voice, clear line: “Your care continues. Your information stays private unless there’s a judge-signed order.”
Then get back to clinical tasks.
- Save your quick tools
Admin/legal number in your phone favorites
A posted “nonpublic area” sign on unit doors
A one-page log at the station for these encounters
A pocket card with your two-line script
- After it’s over, huddle for two minutes
What happened, what worked, what to tweak.
Update the one-pager if needed so the next shift is ready.
For charge nurses and managers:
- Post a one-pager: who to call, what counts as nonpublic, where to log.
- Run a 5-minute drill once a week. New grads included.
- Keep a template note in the EHR for documenting these events.
Our Final Thoughts
You can control the boundary at your door, the calm in your voice, and the safety of the room.
